Wednesday, December 28, 2011
Saturday, December 17, 2011
OCD Workshops for Parents at the Child Mind Institute in New York City
The Child Mind Institute let me know that they are offering a series of workshops for parents of children with OCD, with the last three being in January, February and March, 2012. All of the workshops in the series are free and open to the public. Here's a description of their mission:
Our Obsessive-Compulsive Disorder Parent Support and Information Group workshop series covers a range of issues affecting children with obsessive-compulsive disorder (OCD) and their support networks, from navigating friendships and family gatherings to the ins and outs of treatment and medication. This program is an opportunity to gain invaluable skills and learn how to help your children take control of their condition and thrive. Below you'll find the dates and topics of the 2011-2012 workshops; descriptions to follow.
This series is brought to you by the Child Mind Institute's Intensive Pediatric OCD Program. All workshops are held at the Child Mind Institute headquarters located at 445 Park Avenue (with entrance on 56th Street), New York, NY 10022.
The Nuts and Bolts of Exposure Therapy
Speaker: Jerry Bubrick, PhD, Senior Director, Anxiety & Mood Disorders Center; Director, Intensive Pediatric OCD Program
Date: Tuesday, January 10, 2012
Time: 6:00PM - 7:30PM
Location: Fascitelli Board Room at the Child Mind Institute
At first glance, the treatment for a child with OCD can seem illogical and difficult—why would my child want to do exactly what she fears? In this workshop, Jerry Bubrick, PhD, Senior Director of the Anxiety & Mood Disorders Center and Director of the Child Mind Institute's Intensive Pediatric Obsessive-Compulsive Spectrum Disorders Program explains why exposure therapy is the gold standard in OCD treatment and how it works to alleviate the extreme anxiety a child experiences around his or her symptoms. He explains how to help your child face the "bully in the brain" head-on and regain control over his or her life.
Is Medication Part of the Answer? Medication Approaches to OCD
Speaker: Roy Boorady, MD, Senior Director of the Child Mind Institute's Psychopharmacology Center
Date: Tuesday, February 7, 2012
Time: 6:00PM - 7:30PM
Location: Fascitelli Board Room
When deciding how to best treat a child with OCD, it is important to be aware of all of the options. Treatment for children with OCD will often involve cognitive-behavioral therapy, medication, or a combination of the two. Roy Boorady, MD, Senior Director of the Child Mind Institute's Psychopharmacology Center and one of the nation's foremost experts in the psychopharmacological treatment of children and teens, discusses medication approaches to treating OCD. You'll gain a deeper understanding of when and how medication should be used in the treatment of OCD as well as the benefits and drawbacks of the different classes of medication available.
Real Stories: Parents Speak
Date: Tuesday, March 6, 2012
Time: 6:00 PM - 7:30 PM
Location: Fascitelli Board Room at the Child Mind Institute
Join us for a very special Q&A panel of parents who've successfully led their children through the challenges of OCD. They will share personal stories—their struggles as well as the successes—of raising a child with OCD. You'll have the opportunity to ask questions and gain insight into how you can help your child while maintaining balance in your life.
Wednesday, November 30, 2011
Sunday, November 20, 2011
Back Pain and my OCD.
I put my back out this week. I struggle with the presence of physical pain and the OCD that swoops in to complicate it. The first time I hurt my back, I was all of 24, and visiting my father for vacation. He asked me to vacuum the floor, and by the next morning, I couldn't get upright without my muscles seizing up. I'd never felt anything like it, but I knew that it had to be my imperfection and general deficiency that caused it. Having compassion for myself was not something that came easily, if at all. I had recurring back pain all through my 20's and into my 30's. I did have some physical therapy finally, when I was starting grad school, and the MacKenzie back exercises helped. But I went everywhere with a back pillow, and sat near the aisle so I could go stand up during concerts or lectures. I lived in fear of situations where my back might go out and there would be no way to get relief, or that I would be humiliated by my weakness.
I planned everything around how long I had to sit. I knew where the straight hard chairs were in any place I went to frequently. Once I graduated, and started a new job, my back seized up to the point that I had my husband drop me off a few blocks early to give me a chance to get fully upright before I got to the front door. I was depressed. I was anxious. Once my health insurance started, I went to a physiatrist, and got a referral for more physical therapy. This calmed my back for awhile, but the flare ups continued for a few more years, and then slowly, as I was doing therapy for my depression with Molly, my back stabilized. It seemed like a miracle.
On occasion, my back would get stiff, but recover quickly. But this week, after many situations of uncomfortable chairs--getting my hair washed at the beauty shop(which I do about once a year), meetings, long car trips--and lots of time in the studio, my back protested. I've started my Mackenzie exercises again and that has given me some relief, but I still have 3 more craft shows to get through, and the place I feel worst is in my studio, which is frustrating me, and I feel sad that what I love to do most, make art, is where the pain is aggravated. My OCD is all over this, and the more anxious I feel, the more I do things that make my back hurt even more, rituals of sitting at the computer too long. Slowing myself down is hard. The perfectionism is always in the background shouting about my need to do everything exactly right(whatever that means, since the standard always changes). I am working on it though. And know I may need to go back to the doctor and ask about occupational therapy.
If you have chronic pain and OCD, what helps you? I'd love to hear.
Wednesday, November 16, 2011
Thursday, November 10, 2011
OCD-Stop: Free Online Treatment for OCD in Australia from Swinburne University

I received a message from a research assistant at Swinburne University of Technology in Australia about online treatment they are offering through a study by Swinburne's National eTherapy Centre. Their website mentions Exposure Therapy in conjunction with Cognitive Behavioral Therapy as effective treatment for OCD.
Participants in the trial will be randomly assigned to one of two groups, those undertaking a cognitive behavioural treatment program called Systematic Treatment of Obsessive Compulsive Phenomena or OCD-STOP, and those completing Progressive Relaxation Training. Irrespective of which program they are assigned, all individuals will be given the opportunity to take the alternative treatment at no cost.More about OCD STOP!
OCD STOP! online treatment is based on a face-to-face Cognitive Behaviour Therapy (CBT) already in use. Evidence shows CBT is the most effective treatment for OCD. The online program OCD STOP! is known to help reduce symptoms of OCD. This study aims to find out who can most benefit from this treatment.
OCD STOP is free, safe, completely confidential, and does not use medications.
The 12 week program provides information about OCD, and helps participants learn how to control their anxiety and better manage their OCD. During the trial participants receive assistance in the form of weekly email contact with a qualified therapist.
The director is Prof. Michael Kyrios, an academic clinical psychologist.
Note: OCD Stop! online is free. There is also a group that meets onsite, with a nominal fee.
Swinburne is also offering a 12 week STOP Group for OCD, starting April 2012, at Swinburne's campus in Hawthorne VIC, Melbourne.The program cost $420 for the 12 weeks. You may be eligible to receive Medicare Rebates. Medicare rebates are only available for sessions attended. A Mental Health Care Plan and a GP referral for psychological group therapy are needed to obtain a Medicare rebate for the cost of the group. The next STOP therapy program is planned to commence in April 2012. To find out how you can register to participate in this group please contact the Clinic's Project Officer by phone (03) 9214 5528 or email psychprojects@swin.edu.au
Monday, October 24, 2011
OCD and Serenity
I've been thinking about the Serenity Prayer this week.
God grant me the serenity to accept the things I cannot change, the courage to change the things I can, and the wisdom to know the difference.A lot has been going on and I am dealing with it. My skin biopsy came back benign, and I didn't have the backwash of figuring out whether I'd made a mistake in calling the dermatologist, and being "oversensitive." I took my best guess, and the moment before calling was worst, but I also was accepting that I couldn't diagnose cancer by checking my ear constantly, and that felt so much better than standing in front of the mirror, holding a handmirror and a flashlight and contorting myself to get a glimpse. My mother was back in the hospital for the second time with fluid under her lung, and although I was concerned for her, I didn't research the procedure.
The challenge I always had with the Serenity Prayer is the last line, the "wisdom to know the difference" between what I can and cannot change. In my obsessiveness, I would attempt to definitively figure this out, because I had to be right, or I was a failure as a human being. I had the illusion I actually could have a 100% success rate in predicting whether I could change something, or whether I needed to accept it. Over the last few years of ERP treatment for my OCD, I've come to see that this prayer actually ASKS for the wisdom to know the difference, and this implies that at times we will fail in distinguishing this.
There are some aspects of the 12 Steps that I really resonate with, particularly the idea of life becoming unmanageable when in the power of the disorder. Part of me really hoped that I wouldn't have to deal with uncertain symptoms, health problems, or my mother getting older, and my despair when these things happened was overwhelming. I ritualized to try and make the anxiety go away. Research heart surgery. Research skin cancer. Check my skin. Over and over. But we are embodied creatures, and our bodies are not immortal, and can be injured. The enormity of this is catastrophic when you aren't getting any help for the OCD. The compassion of my therapist, my husband, members of my support group, and blog readers helped me see how much of a burden this can be, and encouraged me to find some kindness for myself.
Wednesday, September 7, 2011
Monday, September 5, 2011
Review of Zelah Green: Who Says I'm a Freak? Young Adult Fiction about OCD
 When the publicist for author Vanessa Curtis contacted me about possibly reviewing the young adult novel, Zelah Green: Who Says I'm a Freak? , I was intrigued, because I was a voracious reader as a teen, but do not recall any books about characters with OCD.
When the publicist for author Vanessa Curtis contacted me about possibly reviewing the young adult novel, Zelah Green: Who Says I'm a Freak? , I was intrigued, because I was a voracious reader as a teen, but do not recall any books about characters with OCD.Zelah is in the confluence of pain between her mother dying, her father remarrying to a woman who doesn't like her, followed by her father disappearing, and her persistent need to keep germs away, and elaborate routines of cleaning, counting and physical gestures. My OCD, although present from age 9 or 10, flared when my father left and my mother was depressed, when I was 16, so I resonated with the overlap of the traumas and the rituals and the flood of anxiety, and the fear of being a freak.
Zelah is from the UK and through various twists in the plot ends up in a group treatment home for teens, run by husband and wife behavior therapists. I don't know how representative this is of the British mental health system, but it does provide a setting for Zelah's growth as she discovers other kids who are "freaks" and finds commonality of experience, and also is guided into exposure therapy for her rituals--purposely touching faucets, and toilets and not washing and moving at an incredibly rapid pace.
My main ambivalence about the book was the tendency of the therapist to dictate what step Zelah would take next in combating her OCD, and her relative quickness in doing what was asked of her. On the other hand, I did appreciate that the therapist understood Zelah's thought process, her fear of bad things happening if she didn't do her routines exactly right, and the focus on addressing the compulsive actions directly, rather than assuming that if everything was made right in her family, then her fears would magically disappear.
I remember at age 13 or 14, noticing that all the young adult novels I read were about unpopular kids, outsiders, with lives in turmoil or chaos. I wondered about that, how the characters seemed on the margins. Of course, I was on the margins as well, and I kept reading the novels, hoping for some company, some acceptance. A book like Vanessa Curtis's could have helped me feel less alone with my anxieties, and my OCD. The closest I came to having this was when I read The Best Little Girl in the World by Steve Levenkron, about a teenage girl with anorexia.
Here is a page from my list of books. I recorded the title of each one, which was probably a compulsion.

Sunday, August 21, 2011
Call for Submissions of Creative Work for OCD Awareness Week 2011: Deadline August 31, 2011
 The IOCDF is asking for submissions of art, writing, music and film for OCD Awareness Week 2011. If you have something you would like to share, the deadline is August 31st, 2011 at 12am EST.
The IOCDF is asking for submissions of art, writing, music and film for OCD Awareness Week 2011. If you have something you would like to share, the deadline is August 31st, 2011 at 12am EST.
What
The International OCD Foundation and its affiliates from across the country will come together to educate their communities and the public as a whole about obsessive compulsive disorder (OCD) and its treatments. Learn from the nation's leading experts about how they work with those who suffer daily from the debilitating disorder. Have the opportunity to hear testimonials from patients both recovering and just beginning treatment and learn about the different treatments and therapies that help people hold jobs, balance relationships with family and friends, and lead more typical and productive lives.
Why
OCD Awareness Week is presented by the International OCD Foundation as a vehicle for support, advocacy and education to help end the stigma surrounding OCD and encourage sufferers to identify the disorder and / or seek treatment. The national Foundation has enlisted the support of its Affiliates nationwide to join in this education effort.
2011 OCD Awareness Week Event - October 15
In an attempt to raise awareness of OCD and effective treatment the IOCDF will hold a national event in Boston, MA this year. This event will be video-streamed live across the country. Building on last year’s successful story telling event this year we will be broadening the event to “creative expression” of OCD. We will be looking for submissions in four different categories (for more specific information pertaining to each category please click on the desired category below):
Click here for applications in the following categories:Casestudy/Artwork
Personal Story/Fiction/Poetry
Short Film/Video/Animation
Song/Music
All submissions will be viewed and judged according to the following criteria:
- Overall quality
- How well it ties into the theme of OCD
- How well it ties into a “Dare to Believe…” theme (read more on the "Dare to Believe" campaign)
Submissions will be accepted between August 1 9am EST until August 31 at 12am EST. Up to 5 finalists from each category (determined by a panel of experts through the IOCDF. The decision of the judges will be final.) will then be posted on our website for the public to vote. In mid-September winners will be announced. Winners will have transportation and hotel accommodations paid for by the IOCDF for the October 15th event.
Click here for applications in the following categories:Casestudy/Artwork
Personal Story/Fiction/Poetry
Short Film/Video/Animation
Song/Music
Friday, August 12, 2011
Free Online Treatment for OCD in Australia

Macquarie University's Centre for Emotional Health in Australia contacted me about passing on information about a free online course they are offering for dealing with OCD. I checked out their About Obsessive Compulsive Disorder (OCD) factsheet, and they advocate for Exposure and Response Prevention Therapy, so if you live in Australia, this could be helpful.
Here are some details:
The eCentreClinic OCD Course is a 5-lesson cognitive and behavioural treatment package that delivers remote evidence- based treatment. The treatment includes techniques that would normally be delivered in face to face treatment. The main emphasis is on exposure and response prevention however the Course also includes a strong cognitive component. The OCD Course is delivered over 8 weeks and the participant has bi-weekly telephone contact with a Clinical Psychologist who is experienced in the treatment of OCD. The Course is open to individuals with all subtypes of obsessive compulsive disorder (with the exception of primary hoarding compulsions).
The OCD Course has been tested in one open trial with 20 participants to date. This research has been accepted for publication in the Journal of Anxiety Disorders. In summary the results from this study showed a high level of acceptability for the Course with 81% of participants completing all the Lessons and 100% of respondents indicating that they would recommend the Course to friends. In terms of clinical outcomes, participants improved significantly on the Yale-Brown Obsessive Compulsive Scale and 52% of participants no longer met criteria for OCD at 3 month follow-up.
Exclusion criteria for the OCD Course include:
- Aged <18
- Primary hoarding compulsions
- Suicidal intent
- History of psychosis
- No access to the internet
- Unstable medication dosage
- Current CBT treatment for OCD
- Residing outside of Australia
For enrollment information, check out The OCD Course.
Saturday, April 23, 2011
Anger and OCD
OCD Reflections had a recent post about White Hot Anger that struck a chord with me, about how she usually keeps her frustration to herself, and if she is angry, it must be fully justifiable, and also gets angry at herself for getting angry. I was the girl who quickly learned that anger was a really bad idea in my family. When my father left he told me I had no reason to be angry, but he was the same person, just in a different context. My parents never fought. I can only remember one disagreement articulated, about whether or not a minor cut needs a bandage, or to fresh air.
This aversion to anger got entangled with my OCD, and when I felt anger, I immediately started analyzing it, trying to figure out if I was justified to feel angry, retracing the conversation, attempting to reconstruct every word. By the time I did this gauntlet of compulsing, the anger was even stronger. One of my feared consequences was that I wouldn't survive feeling angry, that it was dangerous. Another fear was that the anger would never dissipate, and I would be stuck with it forever, haunted by it. Ironically, my compulsions made this come true, by intensifying the feeling.
My ERP therapist told me anger wouldn't kill me, which of course sounded crazy and made me angry. My perfectionism latched onto being angry as "wrong" and I would berate myself for having angry feelings. My therapist told me that feelings just are, that they are just there, and not "justifiable" or "unjustifiable." We can control our actions in response to our anger, or how we view our anger, but if the feeling arises, the more we flee from it, the more it lingers, much like any of my other obsessions. Anger can be a sign that something needs to change, that we feel exploited, or taken advantage of, or hurt, and can give us the energy and motivation to make changes.
The more willing I am to just let the anger be there, as uncomfortable as it is, the less intense it gets. I also need to be willing to guess if I'm angry instead of knowing "for certain" that I am angry--I used to spend a lot of time and energy trying to establish if I was truly angry or not. Anger has set off my OCD in the past, as have just about any strong feelings, negative or positive. But anger was also one of the motivators for my seeking treatment for my OCD, anger at how OCD was eroding my left and affecting my relationships. I met someone who had severe OCD as a child, and if someone tried to interfere with her rituals, she was get extremely angry and lash out. She wasn't able to articulate her fears, or what was going on in her head, and was sent away to a residential school, and it was many years until she was diagnosed with OCD and got treatment, and an understanding that she could survive without her rituals.
How does anger interact with your OCD?
Sunday, April 17, 2011
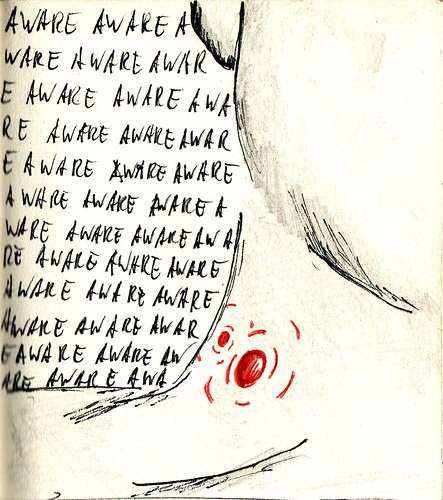
Constantly Aware: OCD, the Body and Health Anxiety
This drawing by fisserman that I found in flickr is very true to my experience of the confluence of body sensations and mental awareness of those sensations, and my OCD. This week I've had tension and twinges in my chest, and my mind latched onto the symptoms. I find it very frustrating how certain bits of dialogue will shoot to the surface, like my doctor asking a few weeks ago if I was having any chest pain when I went in for a blood pressure check. What frustrates me is the almost immediate compulsing about whether I answered her question wrong, or that I have made a mistake, or exactly what do the sensations feel like?
And then I feel temptation to assign meaning to the symptom and the phrases both circulating within in me--a sign? a warning? a condemnation? My feared consequences are multiple, from fear of having a heart attack or dying, to fear of being judged harshly if I turn out to have ignored serious symptoms, and finally the fear that the vigilance about how my body feels will accelerate, get worse, and I will be haunted by the obsession, and that the vigilance will make me notice the sensations more, and it will snowball.
My compulsions range from checking my body--poking at my chest, watching how I sit or stand, to mentally checking my narrative of these sensations, ie. when did they start? What do they feel like? Am I really feeling them? I have resisted the impulse to search on the web, which is one reason this hasn't turned into a full blown OCD crisis, but more of a nagging, gnawing presence. What has helped is knowing that I can't establish what will happen in the future, that it's not my responsibility to do that. If the sensations persist or get worse, I will deal with it then. Or that it's too soon to know if the obsession will haunt me, or pervade everything I do and erode my enjoyment of life. I say this with gritted teeth, but it's true.
I am continuing to do things that I had planned to do, rather than retreating to reading, or otherwise freezing my life while trying to figure out the symptoms. I see my therapist on Thursday, so yay for support! Leonard is the first to say that having body sensations adds a layer of intensity to health anxiety OCD. There's something "there" and it intrudes on consciousness. My best guess is that all the time I'm spending bent over my worktable in my art studio is contributing to tightness in my chest muscles. My OCD would really like to know absolutely for sure that it's not a heart attack, and all the old "you are worthless and despicable" stuff gets mixed in as well, like "you'd better diagnose yourself perfectly or you are unredeemable."
I am feeling better the last couple days. I can tell I'm still vigilant--questions like Will the sensations come back? Get worse? but I know this pattern. I've experienced it many times how certain feelings in my body are more likely to trigger obessions than others. When I get a headache I do not usually obsess I have a brain tumor. If you have a desire to reassure me, I can understand that, but I'd rather hear about how you cope with health anxiety, and what has helped you.
Friday, April 1, 2011
Pure O: How do I tell the difference between obsessions and compulsions?
There's been discussions lately on the OCD support lists about how to tell the difference between an obsession and a compulsion, if it's all thoughts, as in "Pure O." My understanding is that the initial thought is the obsession, and the cascade of thoughts afterwards are the compulsion. For me it would be something like, "What if I said the wrong thing?" as the obsession, followed by trying to figure out if I did indeed say the wrong thing, including retracing my words, trying to account for all of them, which is the compulsion.
The irony is that the compulsion is supposed to be what reduces the anxiety produced by the obsessive thought, and yet, when I used to say "I wish I could stop obsessing about this" what I really meant was the whole flood of compulsions. I fly into compulsing so quickly that it seemed quite dubious that the initial thought was causing the anxiety--surely all the retracing, figuring out, analyzing, and research were the obsession right? How could they possibly be a way to lower my anxiety??
But what I learned during exposure therapy was that compulsions only provide short term relief, and in some cases, very very short term, and then they rebound with their own additional suffering, taking up mental space and energy, and that if I challenged myself to refrain from figuring out an obsessive thought, that my anxiety level immediately spiked, and that was a sign that the compulsion was serving its function of a short term hit of relief, even if I couldn't see it as it happened.
My husband had the flu this week, and he gave this analogy--the virus is the obsession, and the immune system response is the compulsion. When we are sick, what makes us feel lousy isn't the virus itself, but the attack of the immune system on the virus. In the case of our bodies, for the flu or other illnesses, we actually want the immune system to attack, but OCD is more like an allergy, where our immune system attacks something harmless like pollen, mistaking it for an invader. I know the things we obsess about don't seem harmless, and that they are often about things important to us, but our full blown compulsions cause us more misery in many cases than the initial obsession.
In the midst of my worst OCD flare ups, I had glimpses of how destructive the compulsions were, but I was so scared by the obsessive thought that I clung to my compulsions. I finally hit a low point with my health anxiety, that even though I was terrified of getting treatment, I knew I couldn't continue on the way I was going and have any kind of life. If you are like me, you probably also spend time trying to figure out if something is an obsession or a compulsion, and wanting to know for sure which it is. Another lovely complication of the OCD! Take your best guess.
Tuesday, March 15, 2011
My First Dental Filling along with Health Anxiety
I had my dental check up last month, with a new dentist because my old dentist wasn't on the insurance list, and when the dentist called out the number 15 when probing, I knew that couldn't be a good sign. I am in my 40's and never had a cavity. I went home and looked up adult cavities, and stopped after about 10 minutes. In the past I would've searched repeatedly, in hopes of finding the exact answer as to why I had a cavity, and how best to have it filled, so I can tell I've come a long way.
I had it filled yesterday, and there was a whole wave of things to stir up my health anxiety. First, the dentist asks if I want a silver filling or a white filling. I had a moment of "Oh, shit. I have to make a decision. I'm not prepared for this," and I ask what the difference is. He says it's "six of one, half a dozen of the other"--no absolute winner. It's like going to class and discovering a pop quiz and you haven't read the chapter. I picked the silver filling because it was a)cheaper and b)would probably last longer(when I asked which lasted longer the dentist said, "I'm not a fortune teller, but I'd say the silver.") Uncertainty all over the place.
All sorts of tidbits of things I'd heard in the past bubbled up while waiting for the numbing to take effect(what if I'm allergic to novacaine? What if?? What if I chose the wrong thing? What about all those people who are afraid of silver fillings?) I had my knitting which helped, as did thinking of Leonard, and all I've learned from him in Exposure Therapy, and the fact that we really aren't fortune tellers. We take our best guess, and sometimes the outcome sucks.
The sound of the drill wasn't as bad as I thought it would it would be, though it smelled like burning hair. I was pretty calm until I heard the dentist opening and shutting drawers, because he couldn't find something he needed--he's filling in for the regular dentist who is ill, and never used the item he wanted. So I'm listening to him improvising with the dental assistant with whatever they have on hand. The dentist ended by telling me that if I have some sensitivity to heat or cold, it will go away with time. I wanted to say, "I have OCD. My symptoms don't f-ing go away. . ." but I didn't because I know that there is a chance it will actually go away on its own if I let the fear be there, and go on with my life, rather than researching and checking the tooth constantly with my tongue.
I'm proud of myself that I haven't looked up the potential dire consequences of silver fillings, or a lack of cavity varnish. I woke up today wanting to look it all up because I was getting the insistent, "What if you screwed up? What if the sensitivity in your tooth won't go away?" Because, yes, cold water hurts my tooth. Finally I recognized that it's only the day after the dental work. It's too soon to tell. The OCD wants an answer NOW. But if I try to accelerate the answer to tamp down my fear, I will make it worse. If I repeatedly test the tooth with cold water, it is going to bring it to my attention and not give it a chance to get better. It might not. But I am practicing tolerating that uncertainty. That doesn't mean I like it, but I have things I want to do with my life, and probing my tooth will certainly lead to being stuck in compulsions, rather than making art.
Friday, March 11, 2011
Your Thoughts and Prayers Please for Someone Who Has Helped me Heal
Many of you know how much I've healed during my work with Leonard, my Exposure Therapist for my OCD struggles, and now he needs thoughts and prayers for his own healing. I went for my session yesterday, and another therapist came into the waiting room to tell me that Leonard had tried to call all his clients, but that he must not have gotten to me, and that he was in the hospital. He gave everyone a good scare, but it sounds like he's going to be ok and out of the hospital soon, but he has healing ahead of him, and I'm not sure when he'll be back to seeing clients.
I am so grateful for the compassion and skill of this therapist, and saddened that he is going through this hard time. I also feel for his other clients, especially ones who have just started, or who are in OCD crisis. The rapport between therapist and client is an amazing tool for motivation and growth and courage in facing what we fear. Leonard once told me he felt honored that his clients trusted him with their personal thoughts and fears.
Life by its nature is full of the unexpected, pain and suffering, but also contains joy, love and meaning. In the past, my OCD would go into overdrive trying to figure out the suffering, with compulsive analysis, but I am learning that some questions have no answers, and I am able to live in spite of this. I never thought I'd find someone to help me face my OCD, and it feels like a miracle that I did, and I hope for miracles in Leonard's life too.
Edited to add: I saw Leonard for therapy on Tuesday. He is doing much better, and his tests came out negative, so that was a relief! Thanks again for all the thoughts and prayers.
Saturday, March 5, 2011
The Uncomfortable State of Giving myself Credit
So what is it that I fear will happen if I acknowledge the work I'm doing?
- Even more will be expected of me
- I will fail
- This will prove that I am a worthless human
- I will discover it's not possible to be perfect, and that small steps are acceptable, and I will be faced with a flood of sadness about all the time I've lost to perfectionism
- I won't be able to survive the sadness, because it will haunt me every minute
If you are struggling with perfectionism, please know that it is possible to learn how to exist in the world without a constant striving for the perfect, that happiness is possible. Perfectionism can feel like a sticky film that refuses to be washed off, but it is not invincible. To write something that helps others with OCD is one of the most rewarding experiences I've ever had, and although my OCD clamors that I'm not feeling the gratification "perfectly right and sustained", I can still claim the moments of clarity, of being enough, of being myself.
Wednesday, March 2, 2011
Wednesday, February 23, 2011
Monday, February 21, 2011
15 Minutes at a Time: The FlyLady and Exposure Therapy for OCD
In January, faced with increased difficulty finding things in my house, and general chaos, I remembered reading about the FlyLady, and went to her site. Just going there was an exposure for me, since my perfectionism starting raring up, but what I like about the FlyLady is an explicit acknowledgment of how much of the home clutter chaos stems from this very perfectionism. The fear that you have to do it "right" and all at once, and rip apart every closet and scrub every surface.
She advocates doing 15 minutes at a time, and then stopping. That's the hardest part for me. My perfectionism OCD gets entangled in this, and once I start a task, I feel anxiety at the thought of stopping before the task is done, even if there's no clear ending point, and so I keep going until I exhaust myself and it seems preferable to avoid cleaning at all. For someone with contamination OCD the feared consequence may be that nothing is clean enough after only 15 minutes.
The FlyLady is practicing a form of Exposure Therapy. She dares her readers to do housework imperfectly, incompletely, incorrectly. The irony of OCD is that it's all about the anxiety not about reality. Avoiding cleaning altogether is not more "perfect" than doing 15 minutes at a time. A refrain on the FlyLady forums is "I've got so much to clean up that 15 minutes isn't enough time." This kind of thinking is part of why I didn't start actually doing exposures right away when I finally found an Exposure Therapist.
I saw the enormity of my compulsions and anxiety, and I wanted to be better immediately because I was in pain, but also because my perfectionist OCD made it seem dangerous to have a learning curve, to proceed slowly, by trial and error, imperfectly, haltingly, erratically. I needed to do things instantly, the first time, or my feared consequence was that I was a worthless failure. Again, the reality is that avoiding learning or taking small steps serves to give a relief from the anxiety of facing the fear, and yet paradoxically, set me even further behind in getting better from my OCD.
What I have learned in therapy is that anything above zero is good. 30 seconds of resisting compulsions is good. 1 minute. 5 minutes. 15 minutes. It's all good. Exposing myself to something I fear, even if it is the least of my fears, is good. Perfectionism says that you either get better all at once, or you don't get better. This doesn't give me my life back. It keeps me trapped in my compulsions. In 15 minute increments I have cleared through the chaos of my house. The FlyLady motto is that you can do anything for 15 minutes, but for 2011 she's challenging us with a new motto: Let's Go for Seven in 2011
Seven minutes on the timer, because 15 minutes can still be too daunting. The FlyLady says that housework done incorrectly still blesses your family, and in the case of debilitating rituals, this is a powerful statement.
Thursday, February 10, 2011
Finding OCD Support Groups
If there isn't a group in your area, there is a link to a manual by Dr. Jonathan Grayson on how to start your own GOAL group. The support group I've attended is modeled on the GOAL group structure of having a time of sharing followed by making a concrete goal for an exposure to do before the next group meeting. It was very helpful to have accountability and support from other people who understood what it's like to have OCD.
Sunday, February 6, 2011
A Shout Out to OCD Reflections: Things I Have Learned The Hard Way
None of my progress in Exposure Therapy has come through being perfect. None of it was perfect. My therapist said this last week, and it has been on my mind. Perfection was not required in order to do my exposures, live my life, get better from OCD. In fact perfection is the enemy of ever getting started. Then I read Fellow OCD Sufferer's latest post, Things I Have Learned the Hard Way. I encourage you to go read it if you haven't already. She's getting at the heart of some really important stuff for those of us who suffer with perfectionism OCD. I especially resonated with this:
The thing that I kind of overlooked was that whole middle part - you know, the part where you have to do the work and you don't like it and you feel like it's "too soon" or "too much" or "not time yet." Yeah, I kind of forgot about that part. . .I overlooked the middle part too. Like Fellow OCD Sufferer, I am an "OCD Nerd" and had read a thesis' worth of information about OCD, and wanted to do my Exposure Therapy perfectly, which delayed me actually doing much in the way of exposures for my perfectionism for almost a year. In spite of muddling along, I am getting better. My therapist would say there is no other way, that perfection is never an option. This is both liberating and scary. The perfectionism chimes in with "Well, if you can get better, then you will REALLY have to be perfect." I am getting better at recognizing all the guises of my perfectionism, and how rickety the arguments are, and how stifling. I am heartened to read posts where a fellow sufferer gets to the heart of the matter, the moment where you move forward, in the midst of all the "not ready" "not yet" "not right" moments.
Waiting for the day when I feel like being "better" to take action, waiting for a time when I'm 100% sure I want to be well and want to do exposure, isn't exactly a sure-fire strategy. In fact, in retrospect, it's almost doomed to fail. It is unlikely that there will come a day when suddenly getting "better" seems easy or completely "right." If that day does come, it probably means that I'm doing something wrong...
Thursday, February 3, 2011
Tuesday, February 1, 2011
The Purpose of Therapy for OCD vs. the Goal of Therapy for OCD
It helped me to connect the pain of doing Exposures with the purpose of doing them. My therapist didn't ask me to do Exposures just for the sake of doing them, or because it was "correct treatment"--he asked me to do them so I could reclaim my life. The first time I met with him, he listened to my history of having OCD, and said that OCD was a disrespecter of my person. I was struck by this. Much of what is important to me was lost inside the OCD. Connecting with what I value, love, am passionate about, gives me motivation to do my Exposures. I love making art, and this often gives me the fuel to defy the OCD pull toward compulsing, and therefore losing many hours in my day to rituals.
Jeff Bell, IOCDF Spokesman, in his new book When in Doubt, Make Belief: An OCD-Inspired Approach to Living with Uncertainty, argues that human beings are motivated by what they value, by making a difference, and doing things for the greater good:
As seen through the distorted lens of unhealthy doubt, "good"Some of the choices that I want to make, cause me anxiety, and my OCD tendency would be to label them bad, and this crashes directly into an essential part of my soul that knows I want to make these choices, that there are things I want in this life, things I desire to accomplish and experience. With OCD it's hard to inhabit your own life. When I think about all I've lost to compulsions, I feel a deep grief, but every Exposure I do allows me to move back into my own life.
choices are those that reduce our anxiety, while "bad" choices are
those that increase our fear and introduce uncertainty.
What are some good choices that you've made that *increased* your anxiety, but which you chose anyway, because they were in the service of something important to you?
Related:
Jeff Bell's Memoir Rewind, Replay, Repeat
What do you want your life to be about? Action and Commitment Therapy for OCD
Thursday, January 27, 2011
Skype for OCD Study: Project SOS from Drexel University(Residents from PA, NJ, NY, ID, MD, CO, HI, IA, SD, WA, WV and WI may be eligible)
I was contacted by Project SOS of Drexel University, asking if I would advertise their study comparing two different types of Cognitive Behavioral Therapy/Exposure Therapy, administered via Skype. I am glad to pass on this information, and am glad that Drexel is funding research that examines factors related to the dissemination of effective, evidence based treatments for anxiety disorders.
Online Treatment Program for Obsessive Compulsive Disorder
Skype for OCD Study (Project S.O.S.)
General Study Information
Drexel University Anxiety Treatment and Research Program is providing treatment free of charge to eligible participants through the University's Department of Psychology. The research study seeks to examine the effectiveness of two variations of a specific type of Cognitive Behavior Therapy (i.e., Exposure and Ritual Prevention) for people with OCD. Treatment is delivered over a period of 16-18 sessions conducted via the videoconferencing program Skype.
Determine Eligibility to Enroll in Program
Let us know that you’re interested! To determine if you are eligible, please call (215) 553-7000 or email us at drexel.sos@gmail.com and provide us with your name and telephone number. Alternately, you can complete this contact form. However you choose to contact us, a member of our clinical team will be in touch with you promptly.
Here is our Project SOS Contact Information:
Phone: (215) 553-7000
Fax: (215) 762-4834
Mailing Address:
Anxiety Treatment and Research Program
Drexel University
Mail Stop 988
245 N. 15th Street
Philadelphia, PA 19102-1192
Email Address: drexel.sos@gmail.com
You can learn more about the eligibility process here.
Wednesday, January 26, 2011
Sunday, January 23, 2011
Hypochondria and Health Anxiety OCD
About 15 years ago, I was in graduate school, and I had a sharp pain in my neck, ever so brief, and it didn't even register. Then it happened again when I was feeling more stressed, after having read about a bone marrow donor drive, and immediately assuming I needed to participate, in spite of all my anxieties about needles and surgery. This time, the pain in my neck panicked me. Was I having a stroke? What was wrong? Since the internet was still primitive, I did what I used to do, which was go to the library and look for books in the medical reference section. This time I stumbled across Susan Baur's Hypochondria: Woeful Imaginings. It was like seeing myself in the mirror, through the author's accounts of people in history who suffered from fears about their health.
It wasn't enough to make my OCD vanish, but it did give me a window of understanding about my anxieties about my body, and that other people had similar fears, even though the only other person I knew of with this kind of fear was my mother. Another book I found was about Charles Darwin and his health anxieties. He wrote often about his symptoms and fears. I was fascinated, since he is a larger than life figure in history, and yet so afraid. Recently, I read about another book, The Hypochondriacs: Nine Tormented Lives by Brian Dillon, which includes Charles Darwin, Glenn Gould, Michael Jackson and Andy Warhol.
Although the subtitles of these books are full of doom, I remember how much I suffered with my health fears before I had any ERP treatment. The difference now is that I did get Exposure and Response Prevention Therapy, and it is possible to get better, to move beyond torment and woe. Hypochondria, according to the DSM, includes a component of being convinced you have a disease, in spite of medical tests to the contrary. There are definitely similarities with health anxiety OCD, and some even argue they are really the same thing, but the part that differs for me is that I am never absolutely convinced I have a particular disease, but more that I want complete assurance that I don't have it, and my websearching and checking of my body are compulsions to reduce my anxiety. My obsessiveness also extends to getting stuck on whether I really have hypochondria instead of OCD(!), but I've learned that pursuing the fine distinctions makes me much worse. Paul Salkoviskis has done a lot of work with health anxiety, and he emphasizes that seeking reassurance for symptoms tends to make them worse.
Fear of being labeled as a time wasting hypochondriac in my doctor's office has complicated healthcare for me over the years, and caused a lot of angst. I understand doctors have a lot of pressures and time constraints, but health anxiety causes intense suffering, and can be treated, and the more general practice doctors realize this, the more possibility of alleviating the suffering.
Related Resource:
Jonathan Grayson's Freedom From OCD has a section on hypochondria/health anxiety
Script for Fighting Health Anxiety OCD
Skin Cancer Anxiety: Fear, Vigilance and All or Nothing Thinking
Wednesday, January 19, 2011
Monday, January 17, 2011
Finding a therapist for "Pure O" OCD: 5 Things to Watch Out For
I was in psychodynamic therapy for 6 years with a therapist who said I had OCD, but who didn't have a plan to treat my OCD beyond having me avoid my triggers. Previous to that I had several other therapists who didn't really have a clue about my OCD. Here are some things to watch out for--hopefully this will help you find help more effectively and not have to go through the delay I experienced in finally getting Exposure and Response Prevention(ERP) therapy.
- Affirmations. If a therapist tells you to repeat affirmations about being a good person, good father, good teacher, good Christian, good whatever, in order to counteract scary, violent, disturbing thoughts, this just feeds the fire, prompting ever more desperation in trying to prove it to yourself that you are not a monster or a danger to others. This is different from having a compassionate therapist who asserts your value as a human being and encourages you to take your life back from the OCD and any other negative deeply held beliefs about your worth, by doing exposure therapy.
- Deeper Issues. If a therapist tells you there are deeper issues you need to deal with, and then somehow your OCD thoughts will resolve or disappear once you've dealt with the issues, you can be in for a long long stint of therapy. Yes, there may be deep issues in your life, but resolving them is not a treatment for OCD, since the compulsions often complicate any attempts at resolution, and even if you gain a deeper understanding of your psyche, OCD can be incredibly resistant to magically disappearing.
- Thought Stopping. Snapping a rubber band everytime you have an unwanted thought, or imagining a giant stop sign will sensitize you to the thoughts even more. Mental compulsions, on the other hand, can be stopped(even if it seems impossible), which leads to the next point.
- Confusing obsessive thoughts with compulsive thoughts. Pure O isn't pure. I discovered with the help of my ERP therapist, that I have mental compulsions for trying to "undo" my intrusive obsessive thoughts, like freezing(and doing nothing until I solve the issue), retracing my thoughts or actions, analyzing, figuring out, avoiding all reminders of the thought, or researching.
- Disputing the thoughts ad infinitum. Cognitive Behavioral Therapy(CBT) is the larger category that ERP belongs to, but CBT applied to mental obsessions without an understanding of the nature of intrusive thoughts, perfectionism and "just right" feeling can turn dysfunctional thought analysis into compulsions. I would get sidetracked into figuring out whether I'd done a thought record thoroughly enough, and even if I disputed all the errors in my thinking, it didn't seem to stick.
Finding a good therapist for OCD in the US and Canada
Wednesday, January 12, 2011
Tuesday, January 11, 2011
1 Year of Exposing OCD!
I began this blog, Exposing OCD, a year ago. I have learned immensely from the process of writing the posts, reading and responding to comments, and in discovering other bloggers who write about the experience of having OCD. I was initially inspired to start a blog when I came across The Beat OCD Blog: Overcoming OCD One Exposure at a Time. The author was blogging anonymously and about doing exposures, and it was like a door opened to the idea that I could write about my experiences as well. I had been writing articles for an OCD newsletter, but it came out only a few times a year, and I'd noticed writing had been helpful for gaining distance from my old patterns. I'd like to give a shout out to The Beat OCD Blogger(or Ann as she now calls herself), and her incredible persistence in doing exposures and reclaiming her life from exhausting OCD rituals and avoidance of the living she really wanted to do.
I wanted to write about my experience doing Exposure and Response Prevention Therapy(ERP), and as a motivator to actually do more exposures. Ironically I started the blog while at work, where my compulsing ate up many of my days, and avoidance was mixed into my other aims. Writing the blog was a distraction, but as readers found my blog, it helped focus my attention on the nature of OCD as a disorder, especially mental obsessions, intrusive thoughts, indecision, perfectionism and health anxiety. OCD is still a mystery to many people, and the most discouraging is how many therapists also find it a mystery, and either don't realize their client has OCD, or doesn't know about ERP. I hope that in some small way I am helping to describe OCD experiences such a way that others can recognize what they may have found impossible to articulate, and to offer hope that it's possible to get better, to be an inhabitant of your own life, rather than living a life of compulsions.
Writing each post was an exposure, since my perfectionism often had resulted in avoiding writing anything unless it was "perfect," along with fears of saying the wrong thing, or choosing the wrong topic or the incorrect photo. I have been honored by people's willingness to share their own experiences with me by leaving comments on the blog, and encouraged by the number of OCD blogs I've found over the course of the past year. My blog roll has grown, and although I wouldn't wish OCD on anyone, I am thankful for companions for the journey of courage in facing OCD.